Practice of Medicine
article
Reducing the Risk of Medication Errors
Medication errors account for 8% of medical malpractice claims among family practitioners insured by MagMutual. It is estimated that about 50% of medication errors are due to ordering issues, including wrong medication, wrong dose or wrong route.1
To help family practitioners reduce the number of medication errors, MagMutual’s medical faculty and risk consultants have analyzed our claims data, determined the main causes of related claims and developed strategies to improve patient outcomes.
Top Risks
The main causes of claims related to medication errors are:
- Failure to Assess Lab/Vital Results
- Failure to Administer Proper Antibiotics Based on Culture Results
- Patient Monitoring Problem
- Provider-to-Patient Communication
Top Strategies for Reduction
Based on these top risk drivers, implementing the following clinical and operational strategies can help you prevent unexpected outcomes and increase defensibility of a medical malpractice claim:
Clinical strategies
- Discuss and document the high-risk side effects of every new medication. Include the reason why the medication is being recommended, how to monitor for signs of an adverse reaction or toxicity, and what to do if symptoms of potentially dangerous reactions develop.
- Schedule appropriate monitoring diagnostic studies when starting a new medication. Examples include Lasix and interval basic metabolic panel, and Warfarin and scheduling CBC to accompany INR check, especially when first starting the medication.
- At every appointment, review patient allergies (or side effects) and all medications (both prescribed and over-the-counter). You or clinical staff could document “medications reconciled” after reviewing all medications.
- When refills come in electronically or telephonically, consider documenting ‘make appointment or needs labs’ to the prescription that is electronically prescribed."
Operational strategies
- For more commonly prescribed medications, create a patient education handout for possible side effects, concerning reactions, monitoring instructions and what to do if side effects or reactions occur.
- Develop clinic protocol for double-checking medication and dosing when it is prescribed or called into a pharmacy. Discourage verbal orders or phone-in prescriptions when possible.
- At every appointment, review patient allergies (or side effects) and all medications (both prescribed and over-the-counter).
- Develop instruction sheets for patients, outlining a plan for holding and restarting anticoagulation. Sometimes the date to restart the medication is unclear, but the patient should understand the plan is to restart the medication when it is safe. When it is based on the surgeon's recommendation after a procedure, make sure the patient knows to clarify the plan with the surgeon when being discharged from the hospital or surgical center. When it is based on a medical condition (like GI bleed), make sure the patient knows to clarify this with the treating physician. A CHADS2 VACS score should be calculated and used in conjunction with ACC guidelines to provide clear decision-making regarding the appropriate use of anticoagulation.
- Opioid prescribing involves conducting a thorough evaluation of the patient's medical history, including any previous substance abuse issues or risk factors for addiction, screening for high-risk sedative hypnotic medication and alcohol use, as well as using prescription drug monitoring programs to identify potential misuse. Additionally, healthcare providers should prescribe the lowest effective dose for the shortest duration necessary, provide education on the risks and side effects of opioids, and explore non-opioid alternatives or multimodal pain management strategies whenever possible. Be aware of the federal and state laws surrounding opioid prescribing for acute pain management.
Other Top Risks
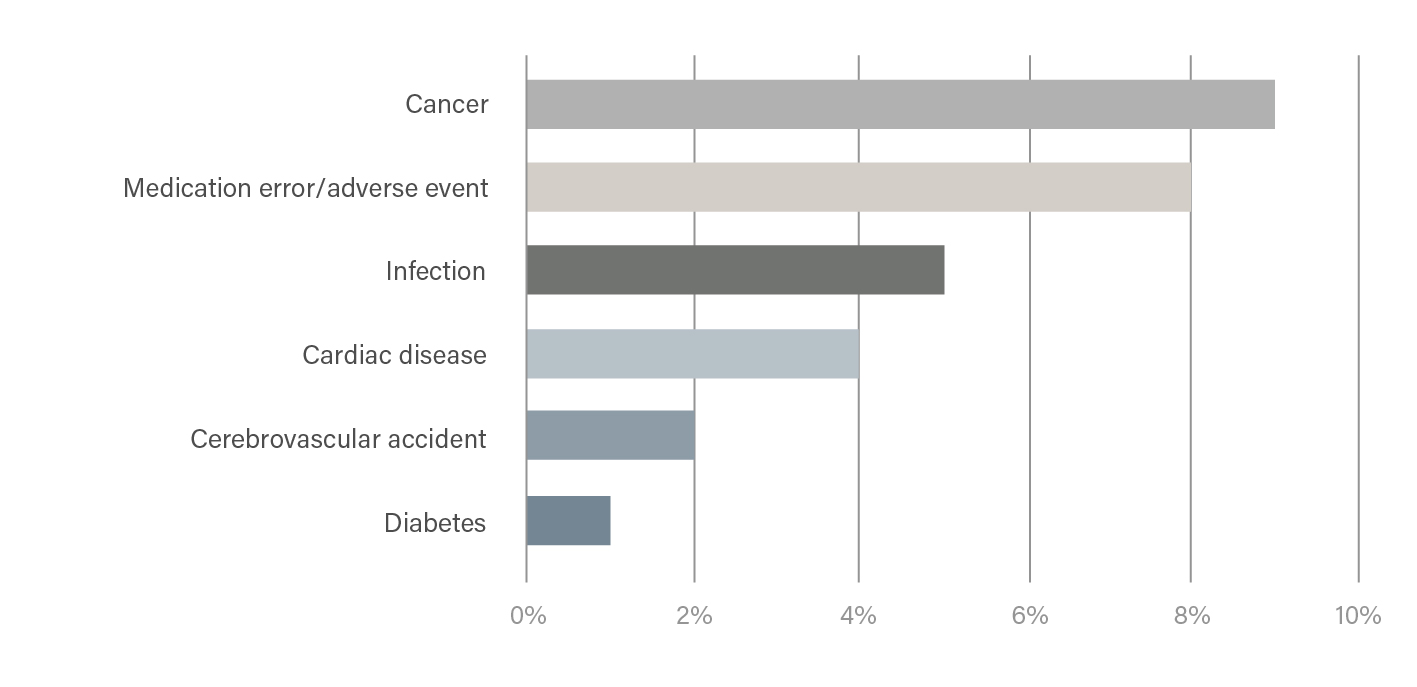
Although medication errors account for many claims among family practitioners according to our data, we’ve identified several other drivers of loss based on claims frequency.
Risk Drivers by Top Cause
| Key Loss Driver | Top Clinical Loss Cause | Top Non-Clinical Contributing Factor | % of Claims |
|---|---|---|---|
| (A) Cancer | Diagnostic | Clinical Systems | 9% |
| (B) Medication error/adverse event | Treatment | Communication | 8% |
| (C) Infection | Diagnostic | Documentation | 7% |
| (D) Cardiac Disease | Diagnostic | Communication | 4% |
| (E) Cerebrovascular accident | Diagnostic | Communication | 2% |
| (F) Diabetes | Treatment | Clinical Systems | 1% |
Risk Drivers by Frequency
Download the full report with indemnity payment information and strategies for all the key loss drivers to help you reduce risk in the top areas that claims occur.
MagMutual PolicyOwners: Log in to view the full report
Not a policyholder? Download Here
Data Collection & Methodology
Data is based on MagMutual closed claims from 2011-2021 and corresponding exposure data. Clinical and non-clinical loss drivers are based on an in-depth review of each claim by a medical professional or clinical risk consultant. Risk reduction strategies are based on input from practicing physicians.
[1] https://www.ncbi.nlm.nih.gov/books/NBK519065/
03/24
Disclaimer
The information provided in this resource does not constitute legal, medical or any other professional advice, nor does it establish a standard of care. This resource has been created as an aid to you in your practice. The ultimate decision on how to use the information provided rests solely with you, the PolicyOwner.